Diffuse Midline Glioma
Brain tumors are the leading cause of cancer death in children. Diffuse midline gliomas are primary central nervous system (CNS) tumors, meaning that they begin in the brain or spinal cord. Diffuse midline glioma is a rare subtype of glial tumors. Diffuse midline gliomas occur in both children and adults. Diffuse midline glioma tends to occur in children, occurring more often in males than females.
Diffuse midline gliomas are all Grade IV tumors; this means they are malignant (cancerous) and fast-growing
An estimated 4600 children per year get brain tumors and about 344 children each year are diagnosed with DMG, with about half having the H3K27M mutation. Most of these kids will die within a year. Roughly 150 kids die each year with this unpredictable, extremely aggressive, mostly undiagnosed and untreatable cancer. While advances have been made across other pediatric cancers such as acute lymphoblastic leukemia (generally fatal 50 years ago with an almost 90% survival rate now), brain tumor survival has not improved over the last 40 years.
Symptoms related to diffuse midline glioma depend on the tumor’s location. People may have double vision, problems swallowing, weakness on one or both sides of the body, or loss of balance. Diffuse midline glioma in the brain also may cause increased pressure within the skull due to production of too much CSF or blockage of its normal flow, known as hydrocephalus. Signs and symptoms of hydrocephalus may include nausea, vomiting, irritability, headaches, blurred or double vision, a strong desire to sleep, and seizures.
Median life expectancy is less than one year. There are no effective therapies if the tumor tissue is not caught early and cannot be removed. Radiation can help extend children’s lives by a few weeks to a few months, but the treatment is excruciating for the patient and the families.
Numerous clinical trials have explored therapies for diffuse midline gliomas; none however, have extended the lifespan of these children beyond radiotherapy mentioned above. Unlike other tumor types, the rare occurrence and eloquent location within the brainstem make obtaining brain tissue difficult and have hampered previous research efforts due to a scarceness of tissue.
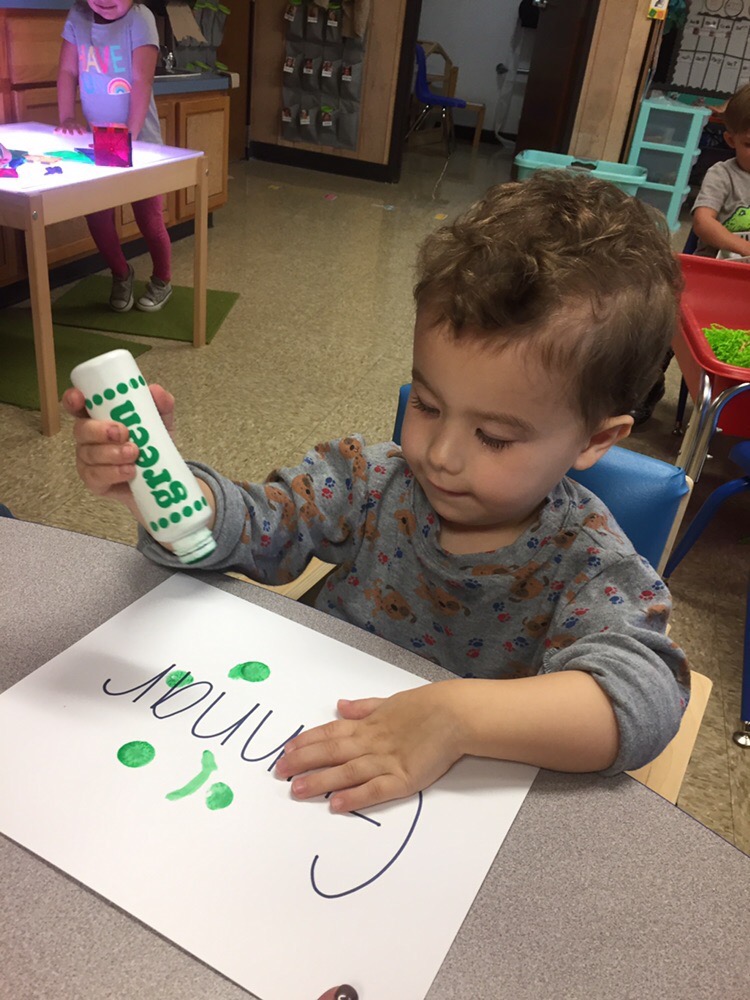
Gunnar was a unique kid. He had his DNA sequenced in life using two methods, his live tumor tissue from the biopsy was sequenced, and we donated his post mortem brain tissue for research. Our hope is that these gifts will help move science forward for predicting, detecting and treating H3K27M DMG and other pediatric brain cancers.